Disease Information
The Function of Bone Marrow
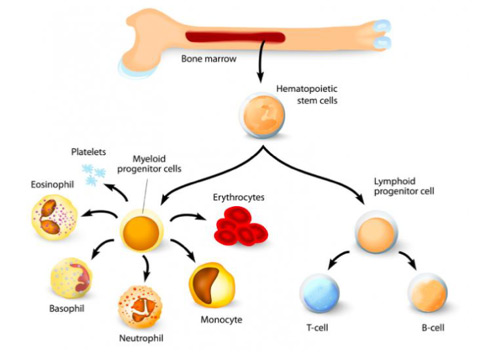
The central portion of bones is filled with a spongy red tissue called bone marrow. The bone marrow is essentially a factory producing the cells of the blood: red cells that carry oxygen from the lungs to all areas of the body; white cells that fight infection by attacking and destroying germs, and platelet cells (platelets) that control bleeding by forming blood clots in areas of injury. Continuous production of blood cells is necessary all through life because each cell has a finite life span once it leaves the bone marrow and enters the blood:
- red cells: 120 days.
- platelets: 8 – 10 days.
- white cells: one day or less.
Aplastic Anemia (AA)
AA is a disease in which the bone marrow stops producing enough blood cells. In AA, stem cells or the marrow microenvironment is defective or damaged, and fails to produce enough blood cells to serve the body’s needs. With prompt and proper care, most patients can be treated. 3,4
Myelodysplastic Syndromes (MDS)
Myelodysplastic syndromes are a family of disorders in which the bone marrow fails to make enough healthy red blood cells, white blood cells and/or platelets. This is because your bone marrow is producing underdeveloped, or immature, cells as well as cells with an abnormal shape, size or look. Most experts agree that MDS is a form of blood and bone marrow cancer. 3,5,8
Paroxysmal Nocturnal Hemoglobinuria (PNH)
Paroxysmal nocturnal hemoglobinuria (PNH) is a rare acquired, life-threatening disease of the blood. The disease is characterized by destruction of red blood cells (hemolytic anemia), blood clots (thrombosis), and impaired bone marrow function (not making enough of the three blood components). PNH affects 1-1.5 persons per million of the population and is primarily a disease of younger adults. The median age of diagnosis is 35-40 years of age, with occasional cases diagnosed in childhood or adolescence. PNH is closely related to aplastic anemia. In fact, up to 30% of newly diagnosed cases of PNH evolve from aplastic anemia. Similarly, the risk of developing PNH after treatment for aplastic anemia with immunosuppressive therapy (anti-thymocyte globulin and cyclosporine) is approximately 20-30%. 3,6,9
Causes of AA, MDS, and PNH
Although a congenital chromosomal abnormality may predispose one to develop inherited aplastic anemia, the medical community does not know the cause of most cases of acquired aplastic anemia. Certain chemicals (such as solvents), environmental toxins (such as certain pesticides), medications, viral infections and radiation exposure appear to cause both myelodysplasia and aplastic anemia, but millions of people with exposure to the same factors do not develop either disease.3-6
The cause of PNH is not known although those with AA have a greater risk of developing the disease.
 Definitions
Definitions
- Erythrocytes – red blood cells
- Neutrophil, Monocyte, Basophil and Eosinophil – white blood cells produced in the bone marrow
- T-cell and B-Cell – also called Lymphocytes