Info sur les maladies
Fonctionnement de la moelle osseuse
La portion centrale des os est occupée par un tissu spongieux de couleur rouge appelé moelle osseuse. La moelle osseuse est essentiellement une usine de fabrication de cellules sanguines : les globules rouges qui transportent l’oxygène à partir des poumons vers toutes les parties du corps, les globules blancs qui luttent contre l’infection en s’attaquant aux organismes pathogènes et en les détruisant et les plaquettes (thrombocytes) qui maîtrisent les saignements en assurant la formation de caillots là où survient une blessure. La fabrication continue des cellules sanguines est nécessaire tout au long de la vie parce que chaque cellule a une durée de vie limitée une fois qu’elle quitte la moelle osseuse pour entrer dans la circulation sanguine :
- globules rouges : 120 jours
- plaquettes : 8 à 10 jours
- globules blancs : un jour ou moins
Anémie aplasique (AA)
L’AA est une maladie caractérisée par l’incapacité de la moelle osseuse à fabriquer suffisamment de cellules sanguines. En présence d’AA, les cellules souches ou le micro-environnement médullaire (de la moelle osseuse) sont défectueux ou endommagés et n’arrivent pas à fabriquer suffisamment de cellules sanguines pour répondre aux besoins de l’organisme. Grâce à un traitement rapide et approprié, la plupart des patients peuvent être soignés3,4.
Syndromes myélodysplasiques (SMD)
Les syndromes myélodysplasiques regroupent diverses maladies caractérisées par l’incapacité de la moelle osseuse à fabriquer suffisamment de globules rouges, de globules blancs et/ou de plaquettes fonctionnels. Cela s’explique du fait que la moelle osseuse fabrique des cellules qui n’arrivent pas à maturité et des cellules ayant une forme, une taille ou une apparence anormales. La plupart des experts considèrent les SMD comme une forme de cancer du sang et de la moelle osseuse. 3,5,8.
Hémoglobinurie paroxystique nocturne (HPN)
L’hémoglobinurie paroxystique nocturne (HPN) est une très grave et rare maladie sanguine acquise. Elle se caractérise par la destruction des globules rouges (anémie hémolytique), la formation de caillots sanguins (thrombose) et une dysfonction de la moelle osseuse (incapacité de fabriquer les trois types de cellules sanguines en quantité suffisante). L’HPN affecte de 1 à 1,5 personne sur un million et est surtout une maladie des adultes jeunes. L’âge médian au moment du diagnostic est de 35 à 40 ans, certains cas étant diagnostiqués durant l’enfance ou l’adolescence. L’HPN est étroitement liée à l’anémie aplasique. En fait, jusqu’à 30 % des nouveaux cas d’HPN diagnostiqués découlent d’une anémie aplasique. De même, le risque de souffrir d’HPN après un traitement immunosuppresseur pour l’anémie aplasique (globuline antithymocyte et cyclosporine) est d’environ 20 à 30 % 3,6,9.
Causes de l'AA, des SMD et de l’HPN
Même si une anomalie chromosomique congénitale peut prédisposer une personne à l’anémie aplasique héréditaire, dans la plupart des cas, la communauté médicale ignore la cause de l’anémie aplasique acquise. Certaines substances chimiques (comme les solvants), les toxines environnementales (comme certains pesticides), certains médicaments ou des infections virales et l’exposition à la radiation semblent causer la myélodysplasie et l’anémie aplasique, mais des millions de personnes qui ont été exposées à de tels facteurs ne présentent ni l’une ni l’autre de ces maladies 3-6.
La cause de l’HPN est inconnue, même si les personnes atteintes d’AA sont exposées à un risque plus grand à l’égard de la maladie.

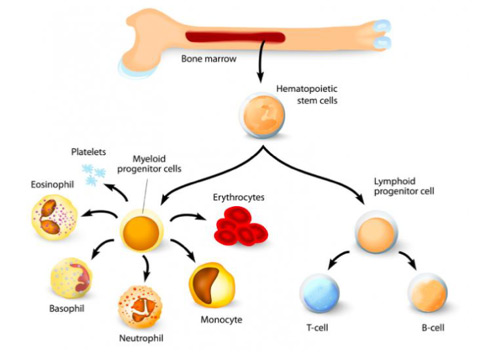
Définitions
- Érythrocytes – globules rouges
- Neutrophiles, monocytes, basophiles et éosinophiles – globules blancs fabriqués dans la moelle osseuse
- Lymphocytes-T et lymphocytes B aussi appelés cellules T et cellules B